建議您使用以下瀏覽器觀看合一網站,
以獲得最佳瀏覽效果。
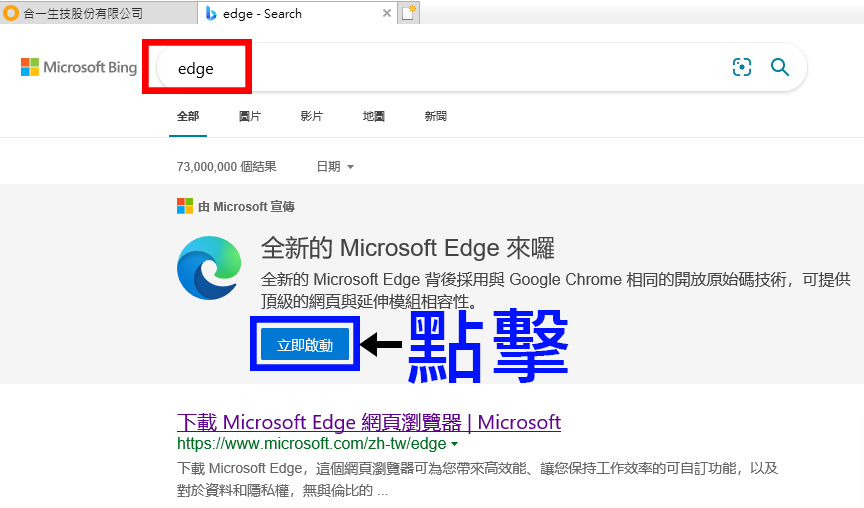
如何使用IE找到Microsoft Edge?
-
開啟新分頁(紅色框)
-
於搜尋框中打入Edge(紅色框),並按搜尋(藍色框)

-
點擊【立即啟動】(藍框處)打開 Microsoft Edge
On Genet’s website, I read an article about the treatment of atopic dermatitis where it said that the Food and Drug Administration approved the marketing of the PDE-4 inhibitor. Does FB-825 work similarly against PDE-4?
1. FB825 is an Anti-CεmX antibody drug; it does not act on PDE4.
2. For PDE4 inhibitors, Crisaborole is the only drug that has been approved by the FDA so far; all the other PDE4 inhibitors are still during their clinical trial phases. These inhibitors are primarily used in patients with mild to moderate atopic dermatitis (EASI<=7, BSA>5%) to reduce symptoms of pruritus and replace topical corticoid steroid (TCSs) and calcineurin inhibiting ointment (TCIs), avoiding side effects of the foregoing two types of ointment when used over an extended period of time.
3. FB825 is mainly used in patients with moderate to severe atopic dermatitis (EASI>=16, BSA > 10%). The two have different target populations.
Regarding the recent oral medication for COVID-19, besides the small molecule drugs from Pfizer and Merck, there seems to be another new nucleic acid drug from Atea Pharmaceuticals, AT-527, which inhibits the replication of the virus at the early stage of infection and reduces the virus to achieve the therapeutic effect. Is this drug based on the same principle as Oneness Biotech’s SNS812? What is Oneness Biotech’s opinion about this new drug?
1. AT-527, Gilead’s Remdesivir, and Merck’s Molnupiravir are all small molecule drugs that are “nucleoside analogue”. These drugs are similar to natural nucleosides and can be misused by the virus’ nucleic acid polymerase, thus preventing the replication of the virus’ genes and achieving the effect of virus inhibition.
2. SNS812 is a siRNA small nucleic acid drug, different from the mechanism of action of the above small molecule drugs. It inhibits the replication of genetic sequences of COVID-19, with high specificity and low off-target rate, and has been shown to be effective and safe in preclinical animal experiments.
How does Oneness Biotech’s SNS812 face the fact that all major international companies have launched therapeutic drugs for COVID-19? Is it already at a disadvantage in terms of timeliness? The Phase I trial will only be conducted next year, so is there any way to get the EUA from FDA?
1. The main drugs for the treatment of COVID-19 that are developing rapidly internationally are “mutagens” and “protease inhibitors”. Viral mutagens have the risk of causing mutations in normal cells of the host, and the actual efficacy and ability of protease inhibitors against variant are yet to be confirmed. SNS812 is a siRNA drug with a different mechanism of action from existing drugs in development. It has specificity and a low off-target rate, and can cover 99.8% of various strains of COVID-19. It has been proven to be safe and effective in preclinical trials.
2. COVID-19 continues to infect and mutate. The future trend is toward the influenzaization of COVID-19 and the coexistence of viruses and humans. The goal of SNS812 is to treat COVID-19, and the development target is positioned as an Oseltamivir (Tamiflu) drug for coronavirus. If the pandemic continues to be severe at the time of completion of Phase II compliance, EUA can be available to market first. If the pandemic has been alleviated and the influenzaization of COVID-19 is formed, it is also in line with the development objective of SNS812 and the development costs will not be unrecoverable. There is no indication that the COVID-19 will disappear.
3. The risk of SNS812 is not whether the development timeline is at a disadvantage, but whether the clinical efficacy is consistent with the effects of preclinical trials. There are many variables in human trials that make it impossible to know whether it will be successful without unblinding.
According to the report, the research team at Agricultural Biotechnology Research Center, Academia Sinica made the discovery through the mice experiments, protein disulfide isomerase a4 (Pdia4) is responsible for regulating the islet cells, and the researched and developed “PS1” inhibits the effect of Pdia4, thus inhibiting the islet failure and reversing the diabetes. This will be the first new target drug for diabetes 100 years after the insulin was invented in 1921. The study has been published in the prestigious international journal “EMBO Molecular Medicine”. The drug is expected to undergo the Phase I clinical trial at the National Taiwan University Hospital early next year and will be on the market seven years later. Does this drug compete with ON101? Is the company interested in seeking the technology transfer?
The causes of diabetes are very complex, and the pancreatic metabolic disorder is only one of them. Many literatures have reported on the relationship between PDIA4 and diabetes. In 2017, the National Defense Medical Center and Tri-Service General Hospital team published the literatures that PDIA4 could be used as a biological indicator for the diagnosis of diabetes. In 2019, Liu et al. also published that PDIA4 gene may play an important role in the pathogenesis of Type 2 diabetes and liver cancer. However, so far PDIA4 has remained a molecular target, and more trials are needed to verify if its inhibitor can reverse the diabetes and become a druggable target.
Pfizer’s abrocitinib for atopic dermatitis was reported to have outperformed the approved drug Dupixent (dupilumab) developed by Sanofi and Regeneron Pharmaceuticals in Phase III clinical data. I wonder if the company has any research on this new drug? Will it affect the cooperation of FB825?
https://geneonline.news/pfizer-atopic-dermatitis-trial/
1. Currently marketed JAK inhibitors, including Eli Lilly’s Olumiant, Pfizer’s Xeljanz, and AbbVie’s Rinvoq, have filed to expand their indications to atopic dermatitis. Nevertheless, there have always been safety concerns about JAK inhibitors. Earlier this year, Pfizer’s Xeljanz was found to increase the risk of heart-related side effects in patients. In July, the U.S. FDA announced a delay in the drug permit license approval of these three JAK inhibitors for atopic dermatitis, to fully and carefully evaluate the safety of JAK inhibitors. In addition, these three JAK inhibitors were required by FDA to add a black box warning on the original package insert, including the increased risk of serious infections, blood clots and cancer.
2. Atopic dermatitis is a chronic disease requiring long-term medication, and the use of oral JAK inhibitors has a high long-term safety risk. Compared with JAK inhibitors, FB825 demonstrated excellent safety in clinical trials in patients with atopic dermatitis. Only the mild to moderate adverse reactions were observed, with no serious adverse reactions. Meanwhile, 67% of patients with FB825 achieved ESAI75 at 16 weeks in the Taiwan exploratory trial, which was administered once every three months. FB825 has a safety advantage similar to that of abrocitinib JAK1 inhibitor taken daily.
Newspapers reported that the research team of Genomic Research Center, Academia Sinica purified and separated the antibodies generated by transgenetic mice vaccinated for 2 doses of monoglycosylated vaccine, found a super antibody, called “m31A7”, with higher affinity than all the monoclonal antibodies on the market, and known from the structure of the super antibody that it can pass all currently known virus mutation variation loci, with stronger binding force with SARS-CoV-2 RBD, which is more than one hundred times better than the current common single strain antibody. If it is put into the clinical treatment in the future, it will be a powerful tool for the treatment of patients.
1. the m31A7 super antibody is successfully developed and marketed in the future, will it be competitive with SNS812?
2. Does Oneness Biotech intend to seek the authorization for clinical trials from Genomic Research Center?
1. Foreign literature has proved that 80% of the novel coronavirus virus mutations occur in the spike protein of the virus. Antibody is a drug that neutralizes the spike protein. Therefore, even if an antibody that can neutralize the current key mutant strains is found through artificial screening, as long as it is an antibody, it will encounter the challenge of high variation of spike protein. SNS812 selected the gene regions that were not mutated from SARS to SARS-COV2 and had a relatively low chance of being affected by viral mutations.
2. The development of new antibody drugs takes a long time and there is no such authorization plan now.
How does your company consider Eli Lilly’s Phase III trial data on atopic dermatitis versus your company’s known data on FB825?
The drug in Eli Lilly’s Phase III trial on atopic dermatitis includes Baricitinib (JAK inhibitor) and Lebrikizumab (IL13 antibody)
1. Baricitinib
Results of Baricitinib Phase III clinical trial (BREEZEAD-AD5) showed that after 16 weeks of treatment in the 2mg daily dose group, 30% of patients achieved EASI-75, compared with 8% in the placebo group. The proportion of patients with an IGA score of 0 or 1 was 24%, compared with 5% in the placebo group.
Due to the concerns about the side effects of JAK inhibitor, the U.S. Food and Drug Administration (U.S. FDA) has once again delayed the drug permit license review of JAK inhibitor and added variables to the drug coming into the market.
2. Lebrikizumab
According to Eli Lilly’s press release, more than 50% of patients achieved EASI-75 in Lebrikizumab Phase III clinical trial. Eli Lilly plans to present the complete Phase III data at the 2022 seminar. In the Phase II trial, the best outcome was 60.6% of patients who achieved EASI-75 after 16 weeks of treatment in the 250mg dose biweekly group, compared with 24.3% in the placebo group. The proportion of patients with an IGA score of 0 or 1 was 44.6%, compared with 15.3% in the placebo group.
3. Data from the exploratory clinical trial of FB825 showed that the proportion of patients who achieved EASI-75 after 16 weeks of treatment with one injection every three months was 66.7%, with minimal adverse drug reactions. In the face of international drug competition, FB825 has advantages in both efficacy and safety.
Is ON101 related to gram-positive bacteria and gram-negative bacteria in the pathogen of diabetic foot infection?
In addition, Centaur Pharmaceuticals launched its new NCE drug WOXheal in India last year. What are the advantages of ON101 compared with WOXheal?
1. The mechanism of action of Fespixon (ON101) is to “inhibit M1-type macrophage inflammatory response, promote M2-type macrophage polarization, reshape the balance of M1/M2 microenvironment of the wound, regulate the wound from inflammation to hyperplasia, and accelerate the wound tissue repair and healing. In contrast to the antibacterial effect of antibiotics against gram-positive bacteria and gram-negative bacteria, according to the International Working Group on the Diabetic Foot (IWGDF) Guidelines, the topical antibacterial agents for skin are not listed in DFU clinical recommendation.
2. This product is a small molecule drug DermaPro developed by CytoTools, a German biotechnology company. The active ingredient is Diperoxochloric acid, and its trade name is WoxHeal in India, with the main effect of antibacterial. The product was previously failed in Phase III clinical trial in Europe (2015), and the technology was transferred to India by Centaur Pharmaceuticals for development. The product was approved for marketing in India in 2019. According to the published clinical data of Phase III in India, the incidence of complete wound closure of diabetic foot ulcer was 71.03%, but the incidence of complete wound closure of active control group (only using the normal saline) was also as high as 57.53%, far higher than the general treatment standard, and the difference between the two groups was 13.5%, p = 0.0156. Due to the lack of published Phase III clinical analysis data, the reliability of clinical efficacy cannot be confirmed.
3. ON101 indications do not restrict the DFU types, and Phase III international multi-center clinical efficacy shows that the difference between ON101 and DFU wound care common dressings Aquacel is 25.57%, p = 0.0001; ON101 Phase III related trial data and mechanism of action have been accepted by internationally renowned SCI Journal, and will be officially released internationally at the beginning of next month (September).
What is the pharmacological effect of the experimental drug FB704A the company expected to be used this year for patients of severe COVID-19 pneumonia? Give an injection or take medicine orally? What is the cost? What is the advantage over the current EUA drugs for COVID-19 pneumonia? What are the advantages compared with domestic competing companies?
1. FB704A is a fully humanized anti-IL6 monoclonal antibody by neutralizing IL6 cytokine and inhibiting the immune trans-signaling pathways of IL6/IL6R to suppress the cytokine storm. The excessive activation of the immune trans-signaling pathways of IL6/IL6R triggers a cytokine storm, which is the main reason for the deterioration of the severe patients. Therefore, it is expected that FB704A can alleviate the deterioration of severe COVID-19 pneumonia.
2. FB704A is currently administered by intravenous infusion, and the dosage form for subcutaneous injection is under development.
3. FB704A is a drug in research and development without the price released yet.
4.Among the EUA drugs currently approved by FDA, Roche’s Actemra (Tocilizumab), already on the market, has the same mechanism of action as FB704A. Preclinical experiments have shown that the advantages of FB704A include: it is a fully humanized antibody with high immunocompatibility; it targets free IL6, ensuring highly safety of human cells; it has a stronger
According to some news reports, the following four companies are also developing drugs for the treatment of coronavirus in Taiwan:
1. Golden Biotech (4132) Antroquinonol (Hocena)
2. Senhwa Biosciences (6492) Silmitasertib (CX-4945)
3. Foresee Pharmaceuticals (6576) MMP-12 inhibitor FP-025
4. TaiwanJ Pharmaceuticals(6549) innovative drugs
Although the information on the drugs of these four companies is hard-to-obtain, can Oneness Biotech make a comparison between SNS812 and the drugs of these four companies?
The mechanisms of action for the 4 drugs are as follows:
As a small molecule kinase inhibitor, Antroquinonol is a drug developed for cancer treatment. According to public information, it can reduce virus replication and viral protein synthesis in cells, thereby preventing organ tissue damage caused by excessive inflammation in mice.
Also a small molecule kinase inhibitor developed for cancer treatment, Silmitasertib inhibits the secretion of virus in infected cells by inhibiting a kinase called CK2, thereby reducing the spread of the virus in the body.
FP-025 is a small molecule inhibitor of MMP-12 (Matrix metalloproteinase-12). Since MMP-12 increases during lung injury or fibrosis and makes the symptoms worse, inhibiting MMP-12 has the potential effect of alleviating the lung symptoms caused by coronavirus and prevent further damage.
As a protease inhibitor for coronavirus, TJC-642 works to interfere with the viral protein and replication functions by inhibiting the viral protease.
In contrast to small molecule drugs or viral protease inhibitors, SNS812 developed by Oneness Biotech is classified as nucleic acid-based drugs. Through the molecular mechanism of RNA interference, SNS812 targets and attacks the gene region where the virus is not prone to mutations, with a high degree of specificity, not susceptible to virus mutation, and a high degree of drug safety.
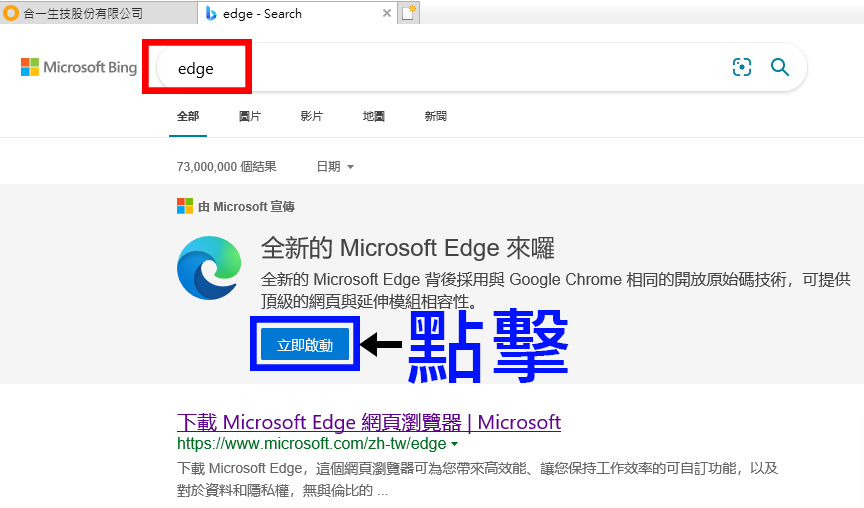
建議您使用以下瀏覽器觀看合一網站,
以獲得最佳瀏覽效果。
如何使用IE找到Microsoft Edge?